Choriocarcinoma: The Notorious “Frightening” Cancer
Choriocarcinoma is a rare type of cancer that develops from the cells that form the placenta during pregnancy. It is a rare but aggressive cancer. Depending on when it develops, there are two main types of choriocarcinoma: gestational (related to pregnancy) and non-gestational (outside of pregnancy). Both types have different progression patterns and outcomes.
This article will focus more on gestational choriocarcinoma, which is more commonly found.
Two Types of Choriocarcinoma
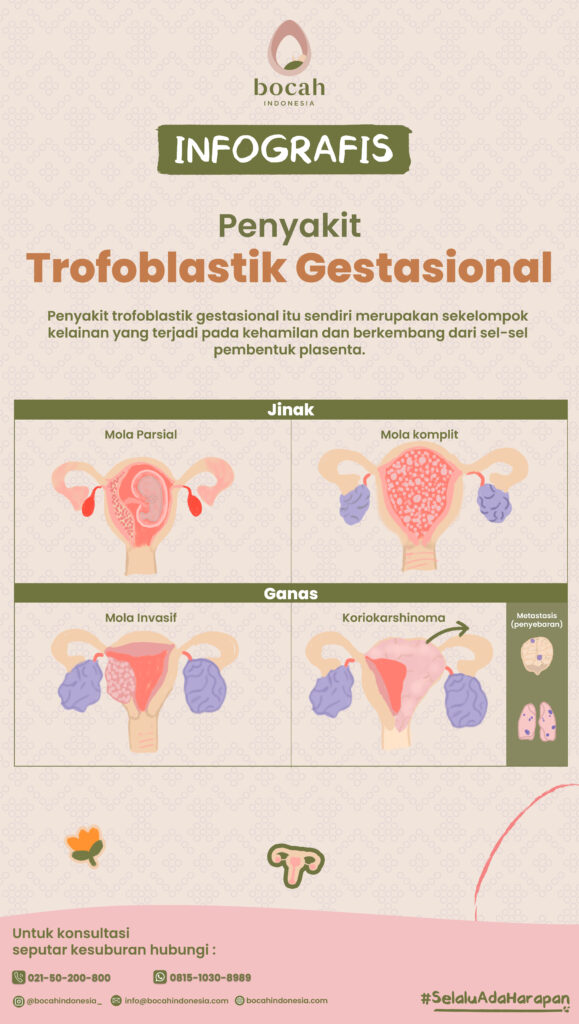
Gestational choriocarcinoma, though more commonly found, is still very rare. The incidence of this type is 1 in 20,000-30,000 pregnancies. This type of choriocarcinoma falls within the spectrum of gestational trophoblastic disease (GTD) and accounts for about 5 percent of all GTD cases. Gestational trophoblastic disease itself refers to a group of disorders that occur during pregnancy and develop from the cells that form the placenta, the organ that provides oxygen and nutrients to the fetus via the umbilical cord.
Gestational choriocarcinoma is more commonly found in women with a molar pregnancy (hydatidiform mole). This cancer can also occur after an ectopic pregnancy, a pregnancy that ends in miscarriage, or even after a full-term normal pregnancy.
The second type of choriocarcinoma, non-gestational, affects both sexes. In this case, choriocarcinoma is a type of germ cell tumor, which arises from the cells that form the human reproductive system. In women, non-gestational choriocarcinoma can develop during prepuberty or postmenopause. The affected organs may be the ovaries or uterine wall, but it does not originate from placental cells. In men, this cancer typically develops between the ages of 15 and 30, affecting the testicles.
Tanya Mincah tentang Promil?
Symptoms of Choriocarcinoma
Women with choriocarcinoma may experience one of the following symptoms:
- Vaginal bleeding: Choriocarcinoma most commonly occurs in the uterus, so vaginal bleeding is the most frequent symptom.
- Abdominal pain or swelling: In rare cases, ovarian cysts may form. This condition causes the abdomen to swell further. Ovarian cysts form due to high levels of the hormone human chorionic gonadotropin (hCG) in the body. Most conditions under the GTD spectrum produce this hormone.
- Anemia or a lack of red blood cells: This condition occurs due to vaginal bleeding.
Choriocarcinoma starts in the uterus but can spread (metastasize) to other parts of the body. The most common site is the lungs, but it can also affect other organs. Here are some symptoms based on the location of cancer spread:
- Lungs: Causes coughing, shortness of breath, and sometimes chest pain.
- Vagina: Causes heavy bleeding or discharge of clots from the vagina.
- Abdomen: Causes abdominal pain, nausea, or vomiting.
- Brain: Causes headaches, dizziness, or seizures.
These symptoms may seem frightening, but choriocarcinoma is almost always curable, even if it has spread to other parts of the body.
Causes of Choriocarcinoma
Gestational choriocarcinoma occurs when the placental cells (trophoblasts) become cancerous. Gestational choriocarcinoma can develop in early pregnancy or after pregnancy. About 50 percent of affected individuals have experienced a molar pregnancy.
In non-gestational choriocarcinoma, cells in the ovaries, testes, or uterus begin to produce the hormone hCG and resemble trophoblasts when viewed under a microscope.
As of now, there is no way to predict when gestational choriocarcinoma will occur. This cancer can develop months or even years after pregnancy. What is certain is that this cancer spreads quickly and is considered one of the more aggressive types of cancer.
Risk Factors for Choriocarcinoma
Gestational choriocarcinoma can occur in anyone who has ever been pregnant, whether the pregnancy was normal, ectopic, or ended in miscarriage. However, studies have found that the highest risk is in women who have experienced a molar pregnancy. Other risk factors include being younger than 20 or older than 40 during pregnancy, using long-term oral contraceptives, and having blood type A.
Complications of Choriocarcinoma
Trophoblastic cells have a strong affinity for blood vessels, meaning cancer cells tend to spread through the bloodstream. Since the lungs have the most blood vessels, they are the most common site of choriocarcinoma metastasis. This also explains why this type of cancer spreads quickly.
Therefore, delaying or not receiving treatment for choriocarcinoma can be fatal. However, with treatment, many choriocarcinoma patients can achieve remission or even be cured. As with most cancers, early treatment leads to the most optimal outcomes.
Diagnosis of Choriocarcinoma
To diagnose choriocarcinoma, the doctor will first conduct a thorough interview. In women, the doctor will pay special attention to reproductive history, particularly miscarriages and molar pregnancies, which increase the risk of choriocarcinoma. In postmenopausal women, any vaginal bleeding should be considered suspicious.
Since choriocarcinoma tends to spread, the doctor will also look for symptoms originating from other organs, such as coughing up blood, shortness of breath, or gastrointestinal bleeding.
To confirm the findings from the interview, the doctor may suggest one or more of the following tests:
- Pelvic examination or physical examination to check for any lumps or masses. In men with choriocarcinoma, the testicles are usually very small or almost absent, with only cancer cells remaining.
- Ultrasound (USG) of the abdomen and pelvic organs.
- Blood tests to determine the level of hCG hormone, which is elevated in choriocarcinoma patients. The increase in this hormone can cause abnormal uterine bleeding, gynecomastia (enlargement of breasts in men), or hyperthyroidism (overactive thyroid).
- Blood tests to check liver and kidney function.
- Complete blood count (CBC).
Once choriocarcinoma is diagnosed, the doctor will evaluate whether there is metastasis or cancer spread to other organs to determine the stage of the disease. For this, the doctor will recommend CT scans of the chest, abdomen, or pelvis, as well as a CT or MRI scan of the head.
Stages of Choriocarcinoma
After choriocarcinoma is diagnosed, the next step is determining the stage of the disease. This step is necessary to understand the extent of cancer spread. The World Health Organization (WHO) and the International Federation of Gynecology and Obstetrics developed a system to determine the stages of choriocarcinoma as follows:
- Stage I: The disease is confined to the uterus.
- Stage II: The disease has spread beyond the uterus but is limited to the genital organs.
- Stage III: The disease has spread to the lungs.
- Stage IV: The disease has spread to other organs.
Next, individuals are classified into low-risk or high-risk groups to determine the treatment they will undergo. The criteria used are as follows:

Treatment of Choriocarcinoma
This cancer is aggressive and often spreads, particularly to the lungs. However, it is highly sensitive to chemotherapy and has a much better cure rate compared to other similar malignant cancers.
The following criteria are generally used to begin chemotherapy for choriocarcinoma:
- Persistent or rising hCG levels after uterine evacuation (curettage).
- Severe vaginal bleeding.
- Gastrointestinal or intra-abdominal bleeding.
- Histological evidence of choriocarcinoma.
- Evidence of spread to the brain, liver, or gastrointestinal tract.
- Lung opacity greater than 2 cm.
- Serum hCG levels above 20,000 IU/L within 4 weeks after uterine evacuation.
- Persistent elevation of hCG levels for 6 months post-evacuation, even if the trend is decreasing.
Chemotherapy agents used are based on the risk assessment at the time of staging.
- Low risk (cumulative score <7) and Stage I-III choriocarcinoma can be treated with single-agent chemotherapy, such as methotrexate or actinomycin D.
- High risk (cumulative score >7) and Stage II-IV choriocarcinoma are treated with multi-agent chemotherapy, additional radiotherapy, and surgery.
After treatment and hCG normalization, hormone levels must be monitored monthly for one year, with two physical exams during that period. If a subsequent pregnancy occurs, a pelvic ultrasound should be performed in the first trimester to ensure the uterine location due to the risk of recurrent choriocarcinoma (although it is rare). Additionally, a placental sample should be taken and examined histologically to determine if there is a recurrence.
Can Choriocarcinoma Be Cured?
In general, choriocarcinoma can be cured with chemotherapy. The outcome is better when the cancer is detected early, before it spreads to organs outside the pelvis. The survival rate for individuals with low-risk gestational choriocarcinoma is nearly 100%. For those with high-risk choriocarcinoma, the survival rate is around 91-94%.
However, non-gestational choriocarcinoma has a much lower cure rate due to being less chemosensitive, meaning chemotherapy may not be effective in killing the cancer cells.
Choriocarcinoma is also harder to cure in cases where:
- The patient has already undergone chemotherapy and it has failed.
- The disease develops after a full-term pregnancy or after childbirth.
- The hCG hormone level is above 40,000 mIU/mL before treatment.
- Symptoms appear, or the patient has been pregnant for more than four months before treatment.
Can You Get Pregnant After Having Choriocarcinoma?
Many women are still able to have children after undergoing choriocarcinoma treatment. However, this depends on the diagnosis and stage of the disease. If you wish to have children, discuss this with your doctor so they can determine the best way to treat choriocarcinoma without affecting your fertility.
Can Choriocarcinoma Be Prevented?
Choriocarcinoma cannot be prevented. However, if you have a history of molar pregnancy, inform your doctor about this risk factor. You should also tell your doctor if you experience unusual vaginal bleeding or lower abdominal pain, especially if you have had a molar pregnancy before.
Source:
- Bishop BN, Edemekong PF. Choriocarcinoma. [Updated 2023 Feb 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. URL: https://www.ncbi.nlm.nih.gov/books/NBK535434/
- Cancer Research UK. (15 Juni 2023). Invasive mole and choriocarcinoma. URL: https://www.cancerresearchuk.org/about-cancer/gestational-trophoblastic-disease-gtd/invasive-mole-choriocarcinoma.
- Cleveland Clinic. (4 Oktober 2023). Choriocarcinoma. URL: https://my.clevelandclinic.org/health/diseases/24863-choriocarcinoma.
- Radiopaedia. (24 Juni 2023). Choriocarcinoma. URL: https://radiopaedia.org/articles/choriocarcinoma-1.