What Is SIS? Understanding Sonohysterography for Uterine Health
Sonohysterography is a non-invasive diagnostic procedure with minimal risk of complications. When complications do occur, the most common is post-procedural infection.
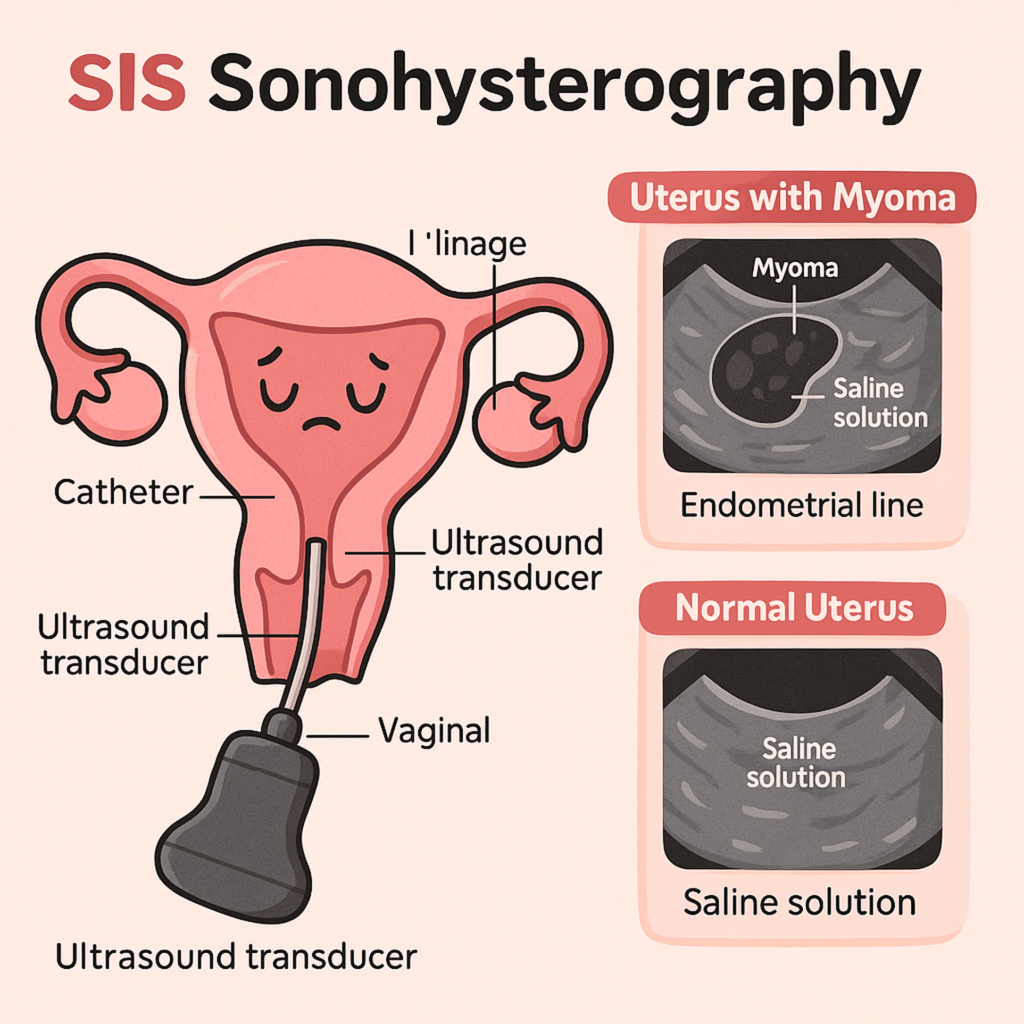
Also known as SIS (Saline Infusion Sonohysterography), this procedure is used to examine the inside of the uterus, specifically the shape of the uterine cavity. In general, SIS aims to detect various abnormalities such as intrauterine fibroids, uterine septa, or tissue adhesions. It is considered a safe examination because it does not involve radiation. Instead, SIS uses sterile saline solution, sound waves, and computer technology to generate images.
Purpose and Indications of SIS
SIS is typically used to help diagnose a range of conditions, including:
-
Uterine fibroids
-
Uterine polyps
Mulai Journey of Hope
-
Intrauterine scarring (synechiae)
-
Abnormal uterine shape
-
Uterine cancer
Doctors may recommend SIS if a woman exhibits symptoms suggestive of uterine disorders, such as:
-
Abnormal menstrual bleeding
-
Infertility
-
Recurrent miscarriages
-
Abnormal pelvic exam findings
SIS is especially useful when standard transvaginal ultrasound fails to provide sufficient diagnostic information.
The only contraindications for SIS are: active pelvic infection, confirmed pregnancy, and the presence of an intrauterine device (IUD).
Preparing for the SIS Procedure
SIS does not require special preparation. However, it yields the most accurate results when performed after menstruation has ended, specifically between days 5 and 9 of the menstrual cycle. This timing also minimizes the risk of infection.
On the day of the procedure:
-
Women can eat, drink, and take regular medications as usual.
-
A doctor may recommend taking over-the-counter pain relievers beforehand to reduce discomfort during the procedure.
-
If necessary, prophylactic antibiotics may be prescribed to help prevent infection.
-
It’s advised to wear a sanitary pad (not a tampon), as saline fluid will discharge from the uterus after the procedure.
Patients will be asked to empty their bladder before the exam and wear comfortable clothing that allows easy access to the lower body.
How SIS Is Performed
The procedure involves slowly injecting 10–20 mL of warm sterile saline into the uterine cavity via a catheter. This saline expands the uterus, allowing clearer imaging with abdominal or transvaginal ultrasound.
Steps of the SIS procedure:
-
After emptying the bladder, the woman changes into a sterile gown and lies on the exam table. No anesthesia is used—patients remain awake. Mild cramping may occur during and after the procedure.
-
A pelvic ultrasound (abdominal or transvaginal) is performed first to assess baseline uterine conditions.
-
A speculum is inserted into the vagina to hold it open and provide visual access to the cervix.
-
The cervix is cleaned with sterile swabs.
-
A thin, flexible catheter is gently inserted into the uterine cavity through the cervix. This may cause a slight pinch or cramping sensation.
-
The speculum is removed while the catheter remains in place. A transvaginal ultrasound probe (transducer) is then inserted into the vagina.
-
The probe, slightly larger than a tampon, is covered with a sterile sheath and lubricated for easier insertion.
-
Through the catheter, 10–20 mL of sterile saline is slowly introduced into the uterus. Cramping may be felt during this step.
-
As the uterus fills with fluid, the ultrasound probe is gently maneuvered to scan and capture detailed images of the uterine lining.
-
The fluid enhances the visualization of the uterine walls, allowing any abnormalities to be clearly detected.
-
Once the imaging is complete, the catheter and ultrasound probe are removed. The saline will gradually drain out of the uterus over the following hours.
SIS is an outpatient procedure and typically takes around 30 minutes, most of which is spent on scanning before and after saline infusion.
What to Expect During and After SIS
Most patients experience little to no discomfort after SIS. Some may report:
-
Mild lower abdominal cramps
-
Spotting or light vaginal discharge
-
Temporary discomfort or fatigue
Cramping, if present, usually subsides within a few hours. Doctors often recommend taking ibuprofen or similar medication beforehand. In some cases, stronger pain relievers or antibiotics may be prescribed.
It is also normal to experience fluid leakage from the vagina post-procedure—this is just the saline used during the SIS, and it may be tinged with a small amount of blood. Leakage may continue for up to 24 hours. Patients may wear sanitary pads but should not use tampons for the rest of the day.
A small number of women may feel lightheaded or dizzy due to cervical stimulation, but this typically resolves within minutes.
Most women can return to their normal activities immediately after the procedure. However, if severe pain, fever, or abnormal discharge occurs in the days following SIS, contact your doctor promptly.
Risks and Complications of SIS
SIS is considered very safe, with serious complications being extremely rare. The main risk is uterine infection, which may present as persistent pelvic pain or foul-smelling discharge. This occurs in fewer than 1% of cases, usually in women who also have blocked or infected fallopian tubes. In such cases, antibiotics are effective.

Advantages and Disadvantages of SIS
Advantages:
-
Superior accuracy in detecting uterine wall abnormalities compared to routine exams
-
Differentiates between abnormalities in the uterine wall vs. endometrium
-
Can assess tubal patency with reasonable precision
-
Minimal time required; outpatient and non-invasive
Disadvantages:
-
May cause temporary discomfort or cramping
-
Slight risk of infection if sterile technique is not strictly followed
-
Less effective than HSG in evaluating the full extent of fallopian tube patency
In infertility evaluations, HSG is often preferred due to its superior ability to visualize the fallopian tubes. However, SIS excels in assessing abnormal uterine bleeding and can serve as a screening tool before proceeding to more advanced imaging like MRI.
Conclusion
Taking cost-effectiveness and diagnostic accuracy into account, Sonohysterography (SIS) is one of the most valuable procedures for evaluating common gynecologic conditions. It is easy to perform, time-efficient, and highly informative—making it a practical and preferred choice in many clinical situations.
Source:
- ACOG Technology Assessment No. 12: Sonohysterography. Obstetrics & Gynecology 128(2):p e38-e42, August 2016.
- American Society of Reproductive Medicine. Saline infusion sonohysterogram. [Revised 2021]. URL: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/saline-infusion-sonohysterogram-shg/#.
- Kumar K, et al. (2023). Utility of Saline Infusion Sonohysterography in Gynecology: A Review Article. Cureus, 15(2), e35424. https://doi.org/10.7759/cureus.35424
- Johns Hopkins Medicine. Sonohysterography. URL: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/sonohysterography#:~:text=Sonohysterography%2C%20also%20called%20a%20saline,a%20baby%20grows%20during%20pregnancy.