Climacteric: Menopause Stage and Hormonal Changes
The Climacteric is a transitional period in a woman’s life that includes the perimenopause phase and several years after menopause.
The Climacteric is a phase of transition between adulthood and old age in a woman’s life. During this period, women go through a stage called menopause, which is the permanent cessation of monthly menstrual cycles. In the climacteric phase, women experience a range of specific symptoms due to significant decline in female hormone levels.
Menopause.
The climacteric is the point at which women who were previously capable of reproduction become non-reproductive. During this phase, the ovaries begin to slow down the process of egg maturation, leading to a depletion of egg quantity, followed by a decline in estrogen levels.
The terms climacteric and menopause are often used interchangeably. However, the term menopause actually refers to a distinct event after a woman has gone through 12 consecutive months without menstruation. Meanwhile, the climacteric is a transitional phase that can last for several years.
Typically, the climacteric starts around 5 years before menopause and may continue until the age of 70. Menopause, on the other hand, usually occurs between the ages of 45 and 55. On average, women experience menopause at the age of 51.
Mulai Journey of Hope
Hormonal changes in women during the climacteric phase
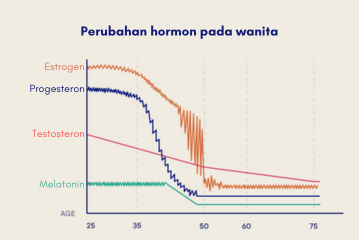
During the transitional phase towards menopause, the production of two major female hormones, estrogen and progesterone, starts to decline progressively. Progesterone decreases first, and its decline is sharp. Estrogen follows a similar trajectory, but its decline is more fluctuating. Meanwhile, testosterone hormone decreases gradually.
Stages of the climacteric:
The climacteric can be divided into three phases based on the gradual and progressive decline in ovarian function:
- Perimenopause: This is the years leading up to menopause. This phase typically starts around 2-3 years (up to 8-10 years) before menopause and ends about one year after the last menstrual period. Signs that a woman is entering the perimenopausal stage include changes in menstrual cycles. Menstrual cycles may become shorter or longer than usual. Menstruation becomes irregular, and the amount of menstrual bleeding may become lighter or heavier. Women may start experiencing the first symptoms of menopause during this phase.
- Menopause: This phase is reached when a woman has gone 12 consecutive months without menstruation. It signifies the end of reproductive years. After menopause, the ovaries stop releasing eggs and cease the production of estrogen hormone.
- Postmenopause: This is the longest phase, lasting between 10 to 20 years. Women will remain in this phase for the rest of their lives. In this phase, cardiovascular diseases, hormonal disorders, and osteoporosis may occur.
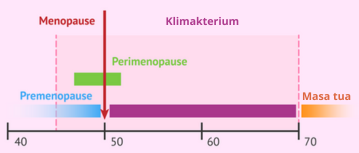
Image source : invitra.com
Symptoms of the climacteric:
There are many symptoms that occur during the climacteric, particularly in the transition towards menopause. These symptoms are primarily caused by significantly reduced estrogen levels. The most common symptoms include:
- Changes in menstrual cycles: Menstruation becomes irregular due to increased levels of follicle-stimulating hormone (FSH) and decreased levels of estrogen and progesterone. While menstruation may be irregular, pregnancy is still possible.
- Hot flashes: Intense sensations of warmth in the body that last for about 2-4 minutes. This is the most common symptom and is triggered by the absence of estrogen, which also regulates body temperature.
- Night sweats: Hot flashes that occur during the night. As a result, women may also experience related symptoms such as fatigue, irritability, forgetfulness, confusion, difficulty focusing, and mood swings.
- Vaginal dryness and urogenital atrophy: This symptom is often accompanied by other symptoms such as vaginal itching, pain during intercourse (dyspareunia), and urinary incontinence. Consequently, women become more prone to urinary tract infections.
- Changes in mood: Women entering the climacteric period often experience psychological symptoms such as feeling easily sad, depressed, difficulty focusing, quick temper, forgetfulness, and others.
- Dry skin: Reduced collagen leads to dry and less elastic skin. This condition makes women more prone to itchiness and skin irritation.
- Joint pain: Hormonal imbalances cause increased stress on joints, tendons, ligaments, and muscles during the climacteric period.
- Weight gain: Decreased estrogen levels affect a woman’s body metabolism. One of the effects is that fat is distributed throughout the body. Basal metabolic rate also decreases, leading to faster weight gain.
- Other common symptoms include migraines, hair loss, brittle nails, decreased libido, facial hair growth, heart palpitations, and reduced memory.
It’s important to note that not all women will experience these symptoms. Approximately 10% of women entering the climacteric phase remain asymptomatic. If symptoms are present, they vary greatly among individuals. Studies show that these symptoms typically start to be felt in the late perimenopause phase and peak in the last two years before menopause, due to a drastic decrease in estrogen levels.
Health risks after menopause:
After menopause, women are at a higher risk of experiencing certain health problems. Some of them include:
- Heart disease and blood vessel disorders: During menopause, the decreased levels of estrogen also lead to a decrease in good cholesterol (HDL). This puts women at an equal risk as men for heart attacks and other blood vessel disorders.
- Osteoporosis: In the early years after menopause, women may experience a rapid loss of bone density. This increases the risk of osteoporosis and fractures, particularly in the spine, hips, and wrists.
- Urinary incontinence: Due to the decreased elasticity of vaginal and urethral tissues, women may experience a strong, frequent, and sudden urge to urinate, accompanied by episodes of involuntary leakage. Urine may also leak during increased abdominal pressure, such as coughing, laughing, or lifting heavy objects. This condition also makes women more susceptible to urinary tract infections.
Considering the aforementioned risks, it is important for women to have regular check-ups with their doctors after entering the climacteric phase.
Are there ways to manage the symptoms of the climacteric phase?
The symptoms and signs of menopause are typically sufficient to indicate that a woman has entered the climacteric phase. If these symptoms are bothersome, there are several ways to reduce the discomfort. Treatment can also be targeted at preventing or managing chronic conditions that occur alongside the aging process.
Treatment options may include:
- Estrogen hormone therapy: This is the most effective way to manage hot flashes. Estrogen is typically given at the lowest dose and for the shortest duration necessary until the symptoms subside. If a woman still has a uterus, estrogen is combined with progestin to prevent thickening of the uterine lining due to estrogen stimulation. Estrogen therapy can also slow down osteoporosis. However, there is an increased risk of breast cancer with long-term hormone therapy.
- Vaginal estrogen: To address vaginal dryness, estrogen can be directly administered to the vagina in the form of creams, tablets, or rings. Topical estrogen can reduce discomfort during sexual intercourse.
- Low-dose antidepressants: Some selective serotonin reuptake inhibitors (SSRIs) can reduce hot flashes. These medications are beneficial for women who cannot undergo estrogen hormone therapy due to medical reasons or who experience mood disturbances.
- Gabapentin: This medication is primarily used for seizures but has shown efficacy in reducing hot flashes. It can be helpful for women who cannot undergo estrogen hormone therapy and experience nighttime hot flashes.
- Medications to prevent or manage osteoporosis: These medications are often combined with vitamin D supplementation to help strengthen bones.
It’s important to discuss the risks and benefits of each therapy with a doctor, as they can vary among individuals. Regular evaluation of the therapy is necessary as needs and treatment options may differ.
Tips for maintaining health during the climacteric phase and after menopause:
The climacteric and menopause are inevitable stages in a woman’s life. Although they may seem uncomfortable, adopting a healthy lifestyle can help women stay healthy and productive in the years leading up to and following menopause. Here are some ways to achieve that:
- Consume a healthy and balanced diet: Limit the intake of fats and sugars to prevent weight gain. Also, limit salt intake as it can increase blood pressure. Ensure an adequate intake of calcium and vitamin D to maintain strong bones.
- Engage in regular exercise and stay active: Regular physical activity not only benefits the body and bones but also helps prevent symptoms of depression. Exercise can include walking, jogging, cycling, yoga, tai chi, and light strength training.
- Maintain a healthy sleep pattern: Establish a regular sleep schedule, waking up and going to bed at approximately the same time each day. Ensure sufficient sleep, aiming for at least 6-8 hours per day.
- Avoid smoking and limit the consumption of alcoholic and caffeinated beverages.
- Undergo an annual medical check-up, including dental and eye examinations.
Equally important, women should seek support from communities of women going through the same phase. Being part of the right community strengthens the understanding that women are not alone during this time and helps maintain positive thoughts and emotions while navigating the climacteric phase.
Disorders that can affect the function of the vas deferens include:
- Congenital abnormalities: Some men are born with incomplete vas deferens, a condition known as congenital absence of vas deferens (CAVD) if only one vas deferens is absent or congenital bilateral absence of vas deferens (CABVD) if both vas deferens are absent. This condition is commonly associated with cystic fibrosis and can cause infertility.
- Vasitis: This condition occurs when the vas deferens thickens due to infection or inflammation of nearby organs. It is also known as deferentitis or funiculitis.
- Blockage: This can occur due to a history of injury or severe infection in the pelvic region.
- Spermatocele: This term refers to cysts that develop above or behind the testes.
- Sexually transmitted infections (STIs): STIs can be acquired through various sexual activities involving the genitals, mouth, or anus.
- Testicular disorders: This includes conditions such as orchitis (inflammation of the testes), testicular cancer, testicular torsion (twisted testicle), and undescended testis.
Although not a disorder, vasectomy procedures affect the function of the vas deferens. This procedure involves cutting and sealing the vas deferens to prevent the release of sperm. It is a highly effective method of contraception (>99.9%) and does not affect sexual function, hormone levels, or other aspects of reproductive and sexual health.
Some symptoms associated with vas deferens disorders include pain, swelling, or lumps in the scrotal area, abnormal penile discharge, azoospermia (absence of sperm) as indicated by semen analysis, and infertility.
- American College of Obstetricians and Gynecologists. [Last reviewed November 2021]. The menopause years. FAQ 047. URL: https://www.acog.org/womens-health/faqs/the-menopause-years.
- Mayo Clinic. [Last reviewed May 25, 2023]. Menopause. URL: https://www.mayoclinic.org/diseases-conditions/menopause/symptoms-causes/syc-20353397.
- Ortmann O, Lattrich C. The treatment of climacteric symptoms. Deutsches Ärzteblatt International. 2012 Apr;109(17):316.
- Taechakraichana N, Jaisamrarn U, Panyakhamlerd K, Chaikittisilpa S, Limpaphayom KK. Climacteric: concept, consequence and care. J Med Assoc Thai. 2002 Jun;85 Suppl 1:S1-15. PMID: 12188398.