Invisible Ovaries, is Fat Tissue a Hindrance?
In some cases, ovaries may not be visible in ultrasound examinations. Find out the reasons here.
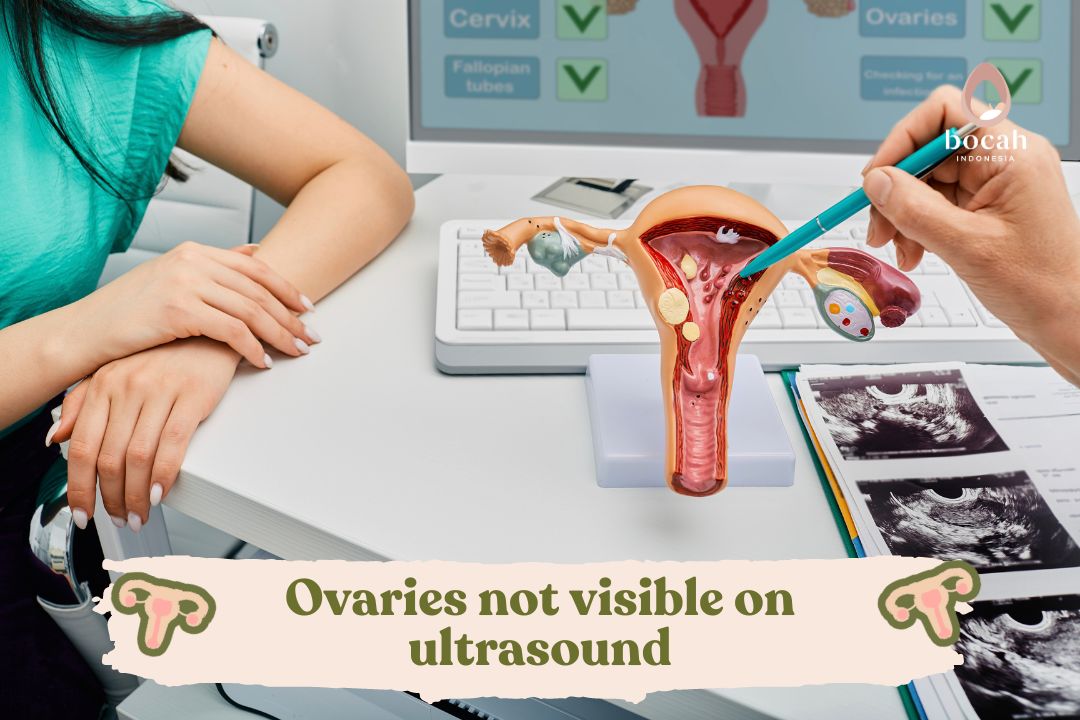
In some cases, the results of the ultrasonography (USG) examination may not clearly show the ovaries. This may raise concerns about health issues.
However, there are implications when ovaries are not visible during USG, one of which is related to menopause. To understand the causes of invisible ovaries in USG and the related issues, read the following discussion.
Ultrasonography (USG) for Ovaries
Women can undergo USG examinations to help assess the condition of the ovaries, including detecting signs of ovarian cancer. There are two common types of USG examinations, namely external USG on the lower abdomen (pelvis) or vaginal USG.
USG examinations use high-frequency sound waves to create images of specific body parts. This examination can display the ovaries, uterus, and surrounding structures.
Tanya Mincah tentang Promil?
In the case of external pelvis USG, the doctor or radiographer will move the probe over the lower abdomen. If the examination is done using vaginal USG, they will insert the probe into the vagina, known as transvaginal USG.
The examination will involve evaluating the ovaries to detect cysts, tumors, or other changes. Additionally, the doctor can also view the uterus, fallopian tubes, and other pelvic structures.
The images produced during the examination will be interpreted by the doctor through consultation. If suspicious findings are present, further examination or recommended treatment actions by the doctor will follow.
Ovary USG examination is a commonly used non-invasive method to evaluate women’s reproductive health and detect abnormalities in the ovaries.
Invisible Ovaries during USG
Ovaries that are not visible during ultrasonography (USG) can be caused by several factors, including:
Closed cervix
The ovaries are located around the uterus, and if the cervix is tightly closed, it can make access to the ovaries difficult during USG examination. In some cases, a closed cervix can hinder the USG probe from reaching and clearly visualizing the ovaries.
Misplaced ovaries
The natural variability in the position of ovaries from one individual to another can be a complicating factor in detecting them during USG examination. Especially in cases where the ovaries are located behind other organs or in a location that is difficult for the USG probe to reach.
Closed adipose tissue
The layer of adipose tissue around the abdomen or pelvis can be a barrier to visualizing the ovaries during USG examination. The presence of fat layers can make it difficult for ultrasonic sound waves to penetrate and reach the ovaries effectively.
If you haven’t had a period in the last 2 years and have entered menopause, the condition of invisible ovaries in USG is generally considered normal. During menopause, ovaries naturally experience a decrease in hormonal activity, and their size may shrink.
Therefore, ovaries that are not visible during USG examination in women who have passed menopause are generally considered part of the physiological changes that occur in the body.
Nevertheless, it is important to always consult with a doctor or healthcare specialist for further evaluation and ensure that there are no underlying medical conditions that need attention.
Ovarian Condition Affects Fertility
The condition of your ovaries significantly influences fertility. This means that the ovarian condition can affect your ability to get pregnant. Ovaries play a crucial role in the menstrual cycle and reproductive process.
Several conditions that can affect fertility through the ovaries include:
Polycystic Ovary Syndrome (PCOS)
PCOS is a condition in which the ovaries produce too much androgen hormones, which can inhibit ovulation or the release of eggs. Women with PCOS may experience irregular menstrual cycles and may find it challenging to conceive quickly.
Endometriosis
Endometriosis occurs when tissue that normally grows inside the uterus (endometrium) grows outside the uterus, including in the ovaries. This can cause cysts, stretching of tissues, and ovulation disturbances, affecting maternal fertility.
Ovulation Disorders
Another relationship between ovaries and maternal fertility is the failure of ovulation, either due to hormonal disturbances or other factors, which can hinder the likelihood of egg and sperm fertilization.
Ovarian Cysts
Ovarian disorders that can be detected in USG examinations include ovarian cysts. If these cysts grow large or are malignant, they can interfere with ovarian function and the ovulation process.
Ovarian Inflammation
If you experience an infection or inflammation in the ovaries, it can damage ovarian tissues and structures, affecting hormonal balance and reproductive function. Some surgical procedures, especially those involving the removal of part or all of the ovaries, can impact reproductive function.
Hormonal Imbalance
Hormonal disorders, such as reproductive hormone imbalances (estrogen, progesterone, and androgen), can disrupt the menstrual cycle and ovulation, hindering the possibility of becoming pregnant.
Early Menopause
In some cases, women may experience menopause earlier or premature menopause. If the ovaries cease normal function earlier than expected, it can lead to early menopause and reduce the likelihood of pregnancy.
The impact of ovarian conditions on fertility can vary. If you are having difficulty getting pregnant or have concerns about your ovarian condition, it is advisable to consult with a doctor or reproductive health specialist for further evaluation and appropriate advice.
Read more information about reproductive health issues and also IVF programs only at Bocah Indonesia.
This article has been medically reviewed by Dr. Chitra Fatimah.
Source:
- Motuzko, Elena, el al. (2018). Non-visualization of the ovary on CT or ultrasound in the ED setting: utility of immediate follow-up imaging. doi: 10.1007/s00261-017-1438-3. https://pubmed.ncbi.nlm.nih.gov/29230555/
- Moorthy rs. Transvaginal sonography. Med j armed forces india. 2017;56(3):181-183. https://pubmed.ncbi.nlm.nih.gov/28790701/
- Petpichetchian C, Pranpanus S, Suntharasaj T, Kor-Anantakul O, Hanprasertpong T. Comparison of transabdominal and transvaginal sonography in the diagnosis of placenta previa. J Clin Ultrasound. 2018;46(6):386-390. https://pubmed.ncbi.nlm.nih.gov/29693718/