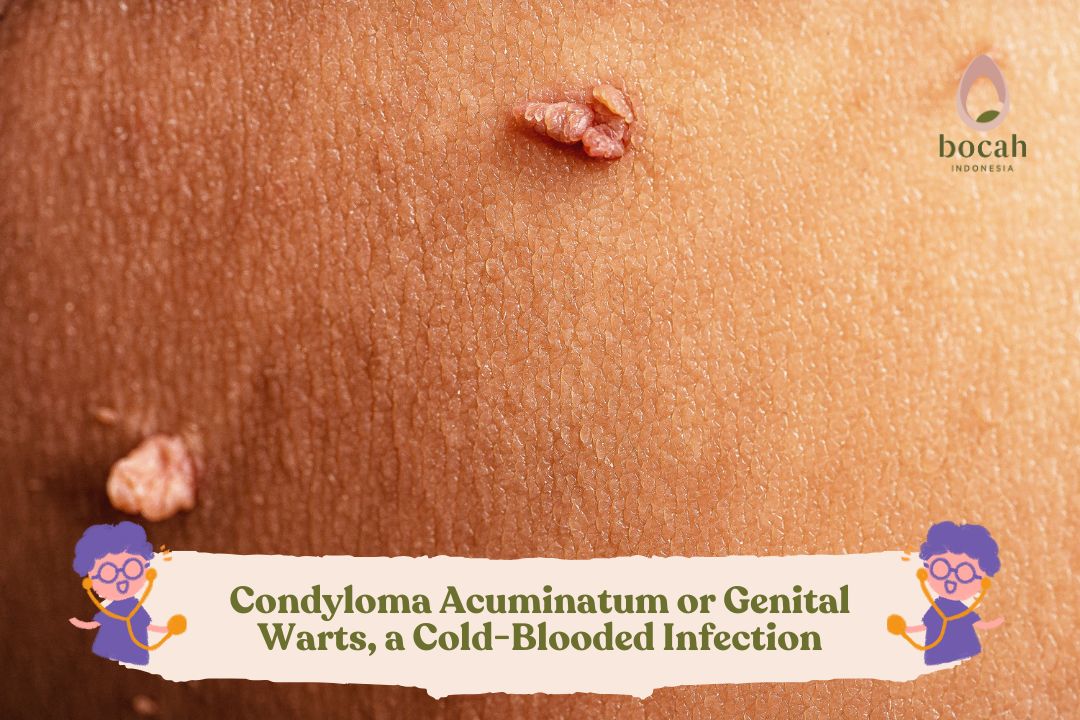
Condyloma Acuminatum or Genital Warts, a “Cold-Blooded” Infection
Genital warts are small, rough bumps that can appear around the vagina, penis, or anus. Medically known as condyloma acuminatum, they are one of the most common types of sexually transmitted infections. The virus that causes them is called the human papillomavirus (HPV). Warts typically appear 3-6 months after infection but can also emerge months or even years later.
Causes of Genital Warts
There are more than 40 types of HPV that can affect the genital area. However, the types most commonly causing genital warts are types 6 and 11.
This virus infects keratinocytes in the skin and epithelial cells on mucous membranes, stimulating their proliferation, leading to visible skin lesions. HPV infection can also be latent or subclinical, meaning it does not develop into visible warts. Such cases can be detected through a Pap smear examination.
Visible genital warts and subclinical HPV infections almost always arise from direct skin-to-skin contact, including:
- Sexual intercourse, which is the most common method of transmission among adults.
- Oral sex.
- Vertical transmission from mother to baby through the birth canal.
- Self-inoculation from one area of the body to another.
Risk Factors for Genital Warts
Most sexually active individuals will be infected with HPV at some point. Therefore, this condition is most commonly found in young adults aged 15-30 years. It is highly contagious. However, genital warts are rare in individuals who have received the HPV vaccination during childhood or adolescence, before becoming sexually active.
Genital warts can also affect infants and young children. The virus can be transmitted during childbirth or through contact with a caregiver’s hands.
Several factors that increase the risk of contracting HPV infection include:
- Not receiving the HPV vaccination.
- Engaging in sexual intercourse without a condom or with multiple sexual partners.
- Having sexual intercourse with a partner whose sexual history is unknown.
- Becoming sexually active at a young age.
- Having a history of other sexually transmitted infections, such as chlamydia or gonorrhea.
- Smoking.
- Having a weakened immune system due to medications that suppress the immune system or as a result of HIV infection.
Symptoms of Genital Warts
Genital warts can grow in the following areas:
Tanya Mincah tentang Promil?
- The vulva or external female genitalia.
- The vaginal walls.
- The perineum, the area between the genitals and the anus.
- The anus and surrounding areas.
- The cervix.
- The head or shaft of the penis.
- The scrotum.
Genital warts can also grow in the mouth or throat of individuals who engage in oral sex with an infected partner.
Symptoms of genital warts include: - Small swellings in the genital area, which may be the same color as the skin or different.
- A cauliflower-like appearance due to clusters of warts growing together.
- Itching or discomfort in the genital area.
- Bleeding during sexual intercourse.
Genital warts can be very small and flat, making them invisible to the naked eye. However, in rare cases, they can grow into large clusters in individuals with weakened immune systems.
Complications of Genital Warts
HPV infection can lead to health issues such as:
- Cancer: Genital HPV infection is closely associated with cervical cancer. Some other types of HPV are also linked to cancers of the vulva, anus, penis, as well as the mouth and throat. Although HPV infection does not always result in cancer, it is crucial for women to undergo regular Pap smears, especially those who have had or are suspected of having high-risk HPV infections.
- Pregnancy complications: During pregnancy, although rare, genital warts can enlarge and make it difficult for women to urinate. Warts on the vaginal walls may obstruct the stretching of vaginal tissues during childbirth. Large warts on the vulva or vagina may bleed as they stretch during delivery. In very rare cases, babies born to mothers with genital warts may also develop warts in their throats, which may require surgery to prevent airway obstruction.
Diagnosis of Genital Warts
Genital warts are usually diagnosed clinically, based on an interview and physical examination. A skin biopsy may sometimes be required to confirm the diagnosis, particularly if there are concerns about cancer.
Some other tests that may be recommended include:
- COBAS 4800 Human Papillomavirus (HrHPV) Test, which can evaluate 14 high-risk (oncogenic/cancer-causing) types of HPV. In certain conditions, the doctor may want to determine whether a dangerous HPV infection is present.
- Pap smear: Sexually active women are advised to undergo regular Pap smears. This test can help detect changes in vaginal or cervical cells caused by genital warts. It can also identify early signs of cervical cancer.
- HPV test: This test aims to detect DNA from specific types of HPV. Only certain HPV types are associated with cervical cancer, with HPV types 16 and 18 being the most common. The sample for this test is usually taken alongside a Pap smear. This test is typically conducted on women aged 30 and above. For younger women, this test is less useful as HPV infections at this age often resolve on their own without treatment.
Treatment of Genital Warts
Genital warts that do not cause discomfort or symptoms are generally left untreated. However, medications or surgery can help alleviate symptoms such as itching, burning, and pain. Treatment can also be beneficial for individuals concerned about spreading the infection.
However, genital warts often reappear after treatment, and there is no cure for the virus itself.
1. Home Treatment
For treatment to be effective, individuals must be able to identify and reach the area with genital warts. After that, follow the medication instructions carefully. Some self-treatment options include:
- Podophyllin solution or cream: Avoid ingesting this solution or cream. This medication is also not recommended for use during pregnancy. Side effects may include mild skin irritation, sores, and pain.
- Imiquimod cream: This cream works by boosting the immune system’s ability to fight genital warts. Avoid sexual contact while the cream is still on the skin, as it can weaken condoms and diaphragms and irritate a sexual partner’s skin. A possible side effect is a change in skin color where the cream is applied. Other side effects may include blisters, pain, coughing, rash, and fatigue.
- Sinecatechins ointment: This ointment can treat genital warts on the body and around the anus. Side effects may include changes in skin color, itching or burning sensations, and pain.
2. Medical Treatment
The medical treatments available in healthcare facilities include:
- Trichloroacetic acid: This chemical treatment will “burn” the genital warts. Side effects may include mild skin irritation, stinging, and pain.
- Podophyllin resin.
- Cryotherapy (freezing with liquid nitrogen): Freezing causes blisters to form around the warts. As the skin heals, the warts will peel off and be replaced by new skin. This method may need to be repeated for optimal results. The main side effects are pain and swelling.
- Electrocautery: This procedure uses electrical currents to burn the warts. Pain and swelling are common post-procedure side effects.
- Surgical removal: Warts can be removed through surgery. Before the procedure, the affected skin area will be numbed with anesthesia to prevent pain. Pain may occur after the procedure.
- Laser therapy: This method uses an intense light beam. Due to its high cost, it is only used for widespread or hard-to-treat warts. Side effects may include scarring and pain.
The above treatments can remove the warts but cannot eliminate the virus that causes them. Warts may also sometimes disappear spontaneously. Conventional theory states that HPV remains in the body for life. However, it is now believed that the virus may disappear or its numbers may be reduced to undetectable levels by PCR tests.
Prevention of Genital Warts
Genital warts are a preventable disease. Some ways to prevent them include:
- HPV vaccination: Currently, the Indonesian Pediatric Society (IDAI), the Indonesian Obstetrics and Gynecology Association (POGI), and the Indonesian Society of Internal Medicine (PAPDI) recommend HPV vaccination for individuals aged 9-26. The vaccine can be given to both girls and boys. It is most ideal and effective when administered to individuals before they become sexually active.
- Staying monogamous: It is safest to have sexual relations with only one partner.
- Using condoms during intercourse: However, this method does not provide 100 percent protection from genital warts. The virus can infect parts of the body that are not covered by the condom.
Conclusion
Around 90 percent of condyloma acuminatum or genital warts cases are caused by HPV types 6 and 11. These types are the least likely to lead to cancer. However, it is still better to prevent HPV infection as there are many types, and several high-risk types can cause cancer.
Source:
- DermNet. (Februari 2021). Anogenital wart. URL: https://dermnetnz.org/topics/anogenital-warts.
- Leslie SW, Sajjad H, Kumar S. Genital Warts. [Updated 2023 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. URL: https://www.ncbi.nlm.nih.gov/books/NBK441884/
- Mayo Clinic. (19 Desember 2023). Genital warts. URL: https://www.mayoclinic.org/diseases-conditions/genital-warts/diagnosis-treatment/drc-20355240.
- Pennycook KB, McCready TA. Condyloma Acuminata. [Updated 2023 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. URL: https://www.ncbi.nlm.nih.gov/books/NBK547667/