3 Common Prostate Problems in Men
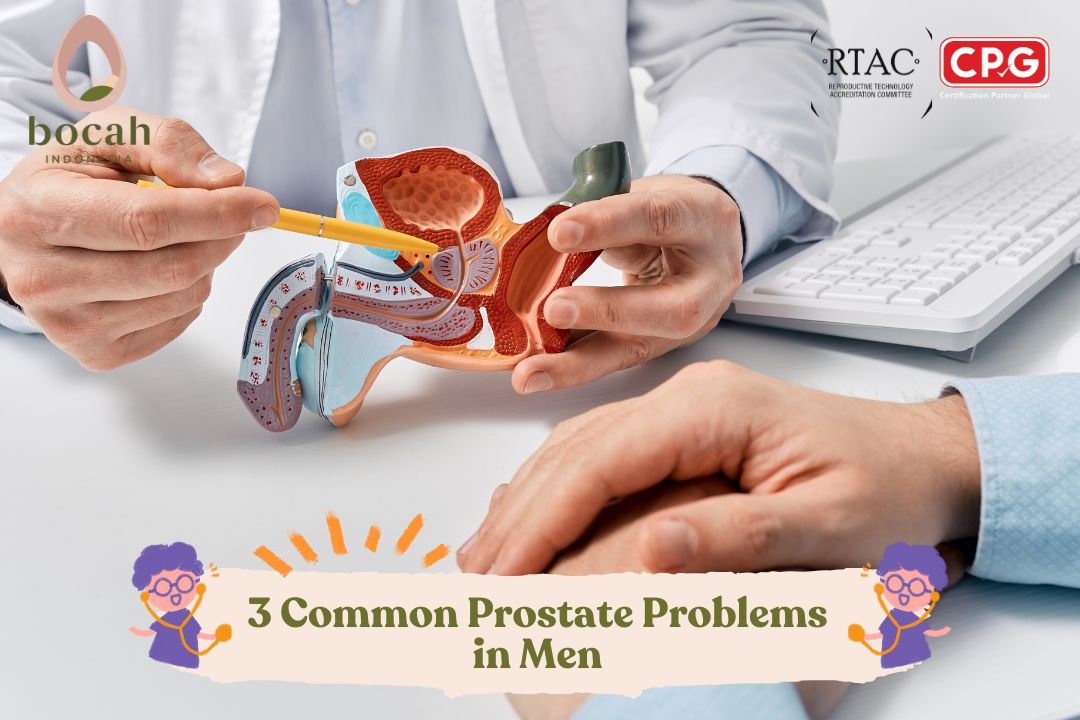
Here are some of the most frequently encountered prostate issues in men.
The prostate gland is a small male organ about the size of a walnut. Despite its modest size, problems can arise if anything goes wrong with it—especially considering its anatomical position relative to other vital structures in the male body.
What Is the Function of the Prostate in Men?
The prostate is part of the male reproductive system, which also includes the penis, scrotum, and testicles. It produces the fluid that forms the bulk of semen, providing nutrients and protection for sperm and enabling them to swim effectively—an essential process for male fertility.
Anatomically, the prostate is located just below the bladder and in front of the rectum. It also surrounds the urethra at the bladder neck—the area where urine exits the bladder. The urethra serves a dual purpose in men, carrying both urine and semen out of the body through the penis during ejaculation.
The prostate has two lobes, right and left, and is broader at the base, which touches the bladder. Its apex is the narrow tip near the rectum. Between the base and the apex lies the central zone of the prostate. Due to its location, any disruption in the prostate can affect urination and sexual function.
Tanya Mincah tentang Promil?
Types of Prostate Disorders
It’s a fact that most men will experience prostate issues at some point in their lives. The three most common prostate-related conditions are:
-
Prostatitis
-
Benign Prostatic Hyperplasia (BPH)
-
Prostate Cancer
1. Prostatitis
Prostatitis refers to inflammation of the prostate gland, and it can affect men of all ages, although it’s most common in men under 50.
There are two primary types:
-
Acute prostatitis, usually caused by a bacterial infection. It leads to sudden and painful urination, weakened urine flow, fever, and chills.
-
Chronic prostatitis, also known as chronic pelvic pain syndrome (CPPS), is a less defined condition. Symptoms may include persistent or recurring pelvic discomfort, burning during urination, increased urinary urgency, incomplete bladder emptying, and painful ejaculation.
The exact cause of chronic prostatitis is often unknown. Possible triggers include:
-
Autoimmune response
-
Undetected bacterial or fungal infections
-
Psychological stress
-
Genital or urinary trauma
-
Repeated prostate biopsies
-
Certain foods and lifestyle habits
2. Benign Prostatic Hyperplasia (BPH)
BPH refers to non-cancerous enlargement of the prostate gland and is the most common prostate issue among men over 50. The prostate may grow two to three times larger as men age. Although not cancerous, BPH can occur alongside cancer.
Approximately half of BPH cases are asymptomatic, but others may experience:
-
Frequent urination, especially at night (nocturia)
-
Weak or intermittent urine stream
-
Hesitancy before urination begins
-
Dribbling or leakage after urination
-
Pain or blood during urination
-
Incomplete bladder emptying
-
Incontinence
-
Straining to urinate
Age is the most significant risk factor for BPH, but other contributing factors include:
-
History of prostatitis
-
Sedentary lifestyle
-
Obesity
-
Hypertension and diabetes
-
Diets high in sugar, red meat, and processed grains
3. Prostate Cancer
Like all cancers, prostate cancer results from abnormal cell growth in the prostate. It can remain localized, spread to nearby tissues (regional), or metastasize to distant organs.
The good news is that early detection, diagnosis, and treatment of prostate cancer have greatly improved in recent years.
Early-stage prostate cancer often shows no symptoms, but advanced stages may present with:
-
Urinary symptoms similar to BPH
-
Visible blood in urine or semen
-
Bone pain
-
Unexplained weight loss
Causes of prostate cancer remain unclear, though genetic mutations (inherited or acquired) play a key role.
Major risk factors include:
-
Age
-
Family history (e.g., a father or brother with prostate cancer increases risk 2–3 times)
-
African-American ethnicity
-
Diets high in red meat and saturated fats
-
Obesity
-
Low ejaculation frequency (as shown in some studies)
Does Prostate Health Affect Male Fertility?
All three prostate conditions described are inflammatory in nature. Inflammation—whether caused by infection, autoimmune response, or other stimuli—can impair prostate function.
The quality of prostatic fluid, which is essential for sperm nourishment and mobility, is a crucial determinant of male fertility. Since the prostate is the main accessory gland of the male reproductive system, local inflammation can directly damage sperm quality and indirectly interfere with reproductive processes.
Conclusion & Prevention
There is currently no guaranteed method to prevent prostate disorders. However, men at higher risk are strongly encouraged to consult a doctor and undergo routine prostate examinations.
It is also vital for men to recognize warning signs—such as difficulty urinating, burning sensation or chills during urination, or visible blood in urine—and seek medical help early to minimize the impact of prostate issues on fertility and overall health.
Source:
- Alshahrani S, McGill J, Agarwal A. Prostatitis and male infertility. Journal of reproductive immunology. 2013 Nov 1;100(1):30-6.
- Motrich RD, Salazar FC, Breser ML, Mackern-Oberti JP, Godoy GJ, Olivera C, Paira DA, Rivero VE. Implications of prostate inflammation on male fertility. Andrologia. 2018 Dec;50(11):e13093. doi: 10.1111/and.13093. PMID: 30569650.
- Verze P, Cai T, Lorenzetti S. The role of the prostate in male fertility, health and disease. Nat Rev Urol. 2016 Jul;13(7):379-86. doi: 10.1038/nrurol.2016.89. Epub 2016 Jun 1. PMID: 27245504.